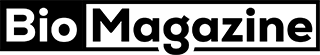
Understanding how to use spirometer properly can significantly improve lung function, accelerate recovery after surgery, and help manage chronic respiratory conditions like asthma and COPD. A spirometer is a simple yet powerful medical device that measures how much air you inhale and exhale, supporting better breathing control and lung expansion.
Healthcare providers frequently recommend spirometer use after surgery, during respiratory therapy, and for long-term pulmonary care. According to the American Lung Association, breathing exercises using spirometry can reduce the risk of post-operative lung complications such as pneumonia and atelectasis.
What Is a Spirometer and Why Proper Usage Matters
A spirometer is a medical breathing device used to measure lung capacity, airflow, and respiratory strength. It is commonly used in hospitals and home care settings to monitor pulmonary health.
Using a spirometer correctly ensures accurate measurement of lung volume and prevents complications such as shallow breathing patterns. It supports oxygen exchange efficiency and promotes alveolar expansion.
Improper technique may reduce effectiveness, delay recovery, and provide misleading lung function results.
Key Benefits of Using a Spirometer
• Improves Lung Expansion and Prevents Collapse
Deep inhalation exercises using a spirometer help open small air sacs (alveoli) that may collapse after surgery or prolonged bed rest. This prevents atelectasis and improves oxygen levels in the bloodstream.
• Reduces Risk of Post-Surgical Pneumonia
After abdominal or chest surgery, patients often take shallow breaths due to discomfort. A spirometer encourages controlled deep breathing, reducing mucus buildup and infection risk.
• Monitors Respiratory Conditions Like Asthma and COPD
Patients with asthma benefit from tracking airflow and lung performance. Regular spirometry helps detect early warning signs of exacerbation.
• Enhances Recovery Speed After Surgery
Studies suggest that consistent use improves oxygenation and reduces hospital stay duration.
• Encourages Proper Breathing Habits
It trains the diaphragm and promotes healthy respiratory muscle strength.
• Provides Measurable Progress Tracking
Visible volume indicators motivate patients by showing lung capacity improvements over time.
Also Read:- How to Use SodaStream: The Complete Expert Guide for Beginners and Advanced Users
How to Use Spirometer Correctly: Step-by-Step Technique
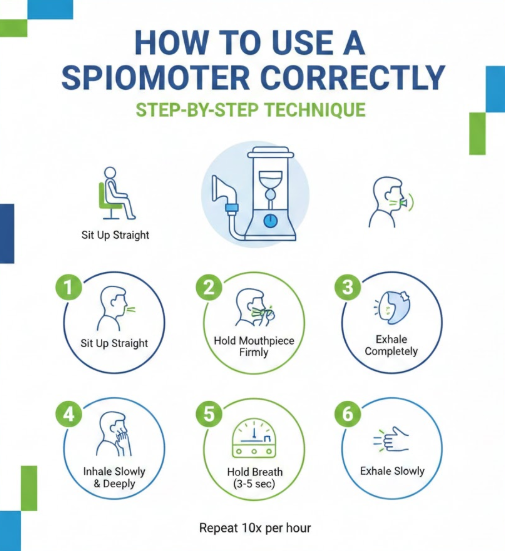
Learning how to use spirometer correctly ensures safe and effective breathing therapy. Proper posture, seal formation, and inhalation technique are critical.
Using correct technique maximizes air intake and lung expansion. Follow the medical guidelines below.
Proper Usage Method
• Sit Upright in a Comfortable Position
Good posture allows full diaphragm expansion. Sit on the edge of a chair or upright in bed with shoulders relaxed.
• Hold the Spirometer at Eye Level
Keeping it upright ensures accurate volume measurement and prevents air leaks.
• Exhale Normally Before Starting
Empty your lungs gently before sealing lips around the mouthpiece.
• Seal Lips Tightly Around the Mouthpiece
A proper seal prevents air escape, ensuring accurate readings.
• Inhale Slowly and Deeply Through the Mouthpiece
Avoid rapid inhalation. Slow, steady breaths expand alveoli effectively.
• Hold Your Breath for 3–5 Seconds
Holding allows air to distribute evenly throughout lung tissues.
Repeat 10 times per session, as recommended by healthcare professionals.
Also Read:- How to Sing: The Complete Expert Guide for Beginners and Advanced Vocalists
How to Use Spirometer After Surgery: Preventing Complications
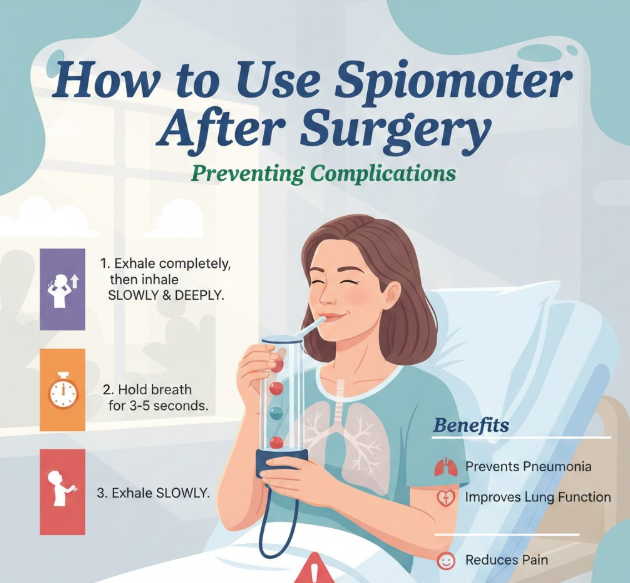
Understanding how to use spirometer after surgery is essential for preventing respiratory complications.
After general anesthesia, lung function may decrease temporarily. Deep breathing exercises restore normal expansion.
Post-Surgery Usage Guidelines
• Start Within 1–2 Hours After Surgery (If Approved)
Early use reduces fluid accumulation and lung collapse.
• Use Every Hour While Awake
Most surgeons recommend 10 repetitions per hour.
• Support Incision with a Pillow While Breathing
This reduces discomfort during deep inhalation.
• Cough Gently After Each Session
Clears mucus and prevents infection.
• Track Daily Progress
Mark volume goals set by your healthcare provider.
• Report Persistent Pain or Dizziness
Consult medical staff if breathing causes discomfort beyond mild strain.
Also Read:- How to Use Shower Oil: The Complete Expert Guide for Silky, Hydrated Skin
How to Use Spirometer at Home: Safe Self-Monitoring

Home spirometry helps patients manage chronic conditions and track lung improvement.
Portable devices are simple to use and require consistent practice.
Home Use Best Practices
• Choose a Clean, Quiet Environment
Avoid distractions to maintain focus.
• Clean Mouthpiece After Each Use
Wash with mild soap and air dry.
• Follow Prescribed Frequency
Typically 3–4 sessions daily.
• Record Your Results in a Logbook
Helps doctors monitor lung function.
• Avoid Using After Heavy Meals
Full stomach may restrict diaphragm movement.
• Replace Device If Damaged
Cracks or leaks reduce accuracy.
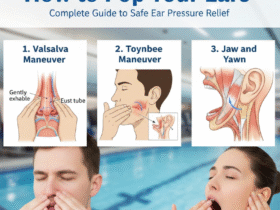
Also Read:- How to Pop Your Ears: Complete Guide to Safe Ear Pressure Relief
How to Use Spirometer for Asthma Management

Patients with asthma benefit from monitoring lung capacity regularly.
Spirometry detects airflow obstruction and helps adjust treatment.
Asthma-Specific Guidance
• Use During Stable Periods for Baseline Readings
Establish normal lung function values.
• Monitor During Symptom Flare-Ups
Detect reduced airflow early.
• Combine With Peak Flow Monitoring
Enhances respiratory tracking.
• Follow Doctor’s Prescribed Frequency
Avoid over-testing.
• Do Not Replace Rescue Inhalers
Spirometer is monitoring tool, not medication.
• Share Results with Healthcare Provider
Improves asthma action plans.
Also Read:- How to Carve a Turkey: The Complete Step-by-Step Expert Guide
How to Use Spirometer Before Surgery: Preparing the Lungs
Using spirometer before surgery strengthens respiratory muscles.
Pre-operative breathing exercises improve surgical outcomes.
Pre-Surgery Preparation Tips
• Begin 1–2 Weeks Before Procedure
Build lung capacity gradually.
• Practice Correct Technique Daily
Consistency improves results.
• Avoid Smoking Before Surgery
Smoking reduces lung elasticity.
• Set Measurable Volume Goals
Monitor daily improvement.
• Consult Anesthesiologist for Instructions
Individual guidance enhances safety.
• Continue Use Immediately After Surgery
Ensures smoother recovery transition.
Also Read:- How to Sell Pokémon Cards: The Complete Expert Guide to Maximizing Value
How to Use Spirometer Device or Machine: Understanding Variations
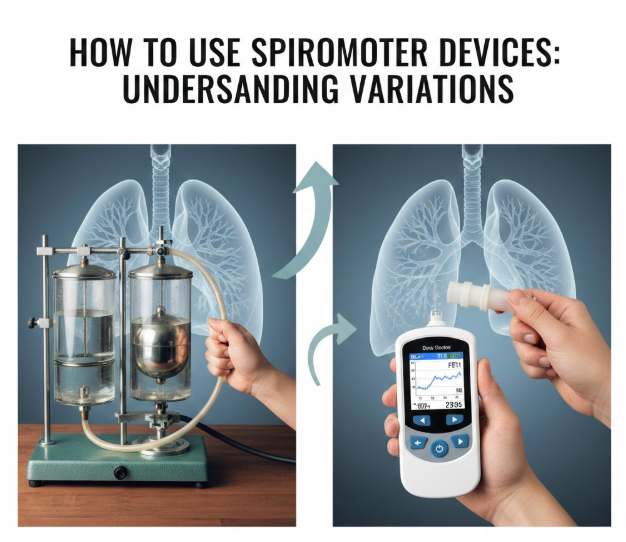
Spirometers come in two primary forms: incentive spirometers and diagnostic spirometer machines used in clinics.
Understanding the difference ensures correct application.
Device vs Machine Differences
• Incentive Spirometer for Home Therapy
Measures inhalation volume visually.
• Diagnostic Spirometer Machine in Clinics
Measures forced expiratory volume (FEV1).
• Professional Testing Requires Supervision
Performed by respiratory therapists.
• Follow Calibration Guidelines
Ensures machine accuracy.
• Avoid Sharing Without Sanitizing
Prevents infection transmission.
• Replace Disposable Components Regularly
Maintains hygiene standards.
Also Read:- How to Sell Gold: The Complete Expert Guide to Getting the Best Value
Cleaning, Maintenance, and Safety Best Practices
Proper cleaning prevents bacterial growth.
Follow manufacturer guidelines for hygiene.
Maintenance Checklist
• Wash Mouthpiece Daily
Use warm water and mild soap.
• Air Dry Completely Before Storage
Prevents mold growth.
• Do Not Submerge Entire Device (Unless Allowed)
Check manufacturer instructions.
• Store in Dry Environment
Avoid humidity exposure.
• Inspect for Cracks or Loose Parts
Replace if necessary.
• Consult Doctor if Dizziness Occurs
Pause use if symptoms arise.
Also Read:- How to Store Peaches: The Complete Expert Guide to Keeping Peaches Fresh Longer
Evidence-Based Benefits of Regular Spirometer Use
Research shows incentive spirometry reduces pulmonary complications post-surgery.
Clinical studies cited by the World Health Organization emphasize respiratory hygiene in preventing hospital-acquired infections.
Benefits include:
• Improved oxygen saturation
• Reduced hospital stays
• Better asthma symptom control
• Strengthened respiratory muscles
• Lower pneumonia rates
• Enhanced breathing awareness
• American Lung Association
• Centers for Disease Control and Prevention
• World Health Organization
• Mayo Clinic respiratory care guidelines
Conclusion
Now you understand how to use spirometer safely and effectively — whether after surgery, at home, for asthma, or before a procedure.
Consistent, correct use promotes lung expansion, prevents complications, and improves respiratory strength. Always follow healthcare provider instructions and maintain hygiene practices.
With proper technique and routine use, spirometry becomes a powerful tool in protecting and improving your lung health.
Also Read:- How to Make a Paper Airplane: The Ultimate Step-by-Step Guide for Distance, Speed, and Fun
FAQs
How often should I use a spirometer?
Typically 10 breaths per hour after surgery, or as prescribed.
Can spirometer use cause dizziness?
Yes, if breathing too quickly. Pause and resume slowly.
Is spirometer useful for COVID recovery?
Yes, under medical supervision for lung rehabilitation.
Can children use spirometers?
Yes, if age-appropriate and supervised.
How long should I continue after surgery?
Usually until mobility increases and lung capacity stabilizes.
For More Updates Visit: Biomagazine
Leave a Reply